Even though we have entered a new year there were plenty of important health news stories from 2015 which we still want to mention. In particular there were many stories regarding multiple sclerosis, chronic pancreatitis and rheumatoid arthritis, just to name a few.
Below are some of those important health news stories which you may have previously missed but luckily we have compiled them together for you to keep you informed.
Multiple sclerosis paroxysmal symptoms confused with seizures due to sudden onset
Advertisement
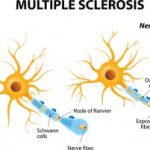 Multiple sclerosis paroxysmal symptoms can be confused with seizures due to its sudden onset. Paroxysmal symptoms are unique to multiple sclerosis (MS) and involve unusual sensations or muscular contractions. The main differences between multiple sclerosis paroxysmal symptoms and epileptic seizures are that paroxysmal symptoms do not cause short-circuiting of brain waves and do not have other features in the brain, such as epileptic seizures.
Multiple sclerosis paroxysmal symptoms can be confused with seizures due to its sudden onset. Paroxysmal symptoms are unique to multiple sclerosis (MS) and involve unusual sensations or muscular contractions. The main differences between multiple sclerosis paroxysmal symptoms and epileptic seizures are that paroxysmal symptoms do not cause short-circuiting of brain waves and do not have other features in the brain, such as epileptic seizures.
Paroxysmal symptoms can be sudden but are short lasting, and if symptoms last for several days, it could be due to exacerbation or relapse. There are many conditions and symptoms that can trigger paroxysmal symptoms, including fatigue, change in temperature, emotional changes, or a sudden change in body position. Continue reading…
Chronic pancreatitis (pancreas inflammation) likely with smoking, alcohol and gene mutation
 Chronic pancreatitis (pancreas inflammation) is likely associated with smoking, alcohol and gene mutation. Chronic pancreatitis is a long-term progressive inflammatory disease of the pancreas, which can lead to permanent damage and malfunction of the pancreas.
Chronic pancreatitis (pancreas inflammation) is likely associated with smoking, alcohol and gene mutation. Chronic pancreatitis is a long-term progressive inflammatory disease of the pancreas, which can lead to permanent damage and malfunction of the pancreas.
The pancreas is an organ located in the abdomen and is responsible for producing enzymes and hormones to help digest and breakdown food. These enzymes and hormones are released into the small intestine and bloodstream to help further break down food from the stomach. The pancreas also produces insulin to help moderate blood sugar levels. In diabetics the pancreas does not work properly and overproduces insulin because the body does not use it properly, leading to high levels of sugar in the body. Continue reading…
Manage rheumatoid arthritis flare-ups during the holiday season
 If you have rheumatoid arthritis the holiday season can be a difficult time. If you encounter a rheumatoid arthritis flare-up during the holidays it can be so painful you may not even wish to partake in any of the festivities simply because you’re in so much pain.
If you have rheumatoid arthritis the holiday season can be a difficult time. If you encounter a rheumatoid arthritis flare-up during the holidays it can be so painful you may not even wish to partake in any of the festivities simply because you’re in so much pain.
A rheumatoid arthritis flare-up is categorized by pain, inflammation, stiffness, fatigue, and impaired physical function which can limit your ability to perform basic, everyday tasks. If not properly managed rheumatoid arthritis flare-ups can really put a damper on your daily life along with your holiday season. This is why it is of utmost importance that you not only take effective measures to manage rheumatoid arthritis for the holidays but for everyday as well so that you are not limited by your condition. Contniue reading…
Hepatitis C virus infection causes rheumatoid arthritis, before HCV detection
 Hepatitis C virus (HCV) infection has been found to cause rheumatoid arthritis, even before HCV is detected. Hepatitis C can contribute to liver failure but is also known to cause rheumatoid arthritis – inflammation of the joints. Due to the link between HCV and rheumatoid conditions, it’s important that newly diagnosed patients of rheumatoid conditions also get tested for HCV as rheumatoid conditions can still occur before HCV is even detected.
Hepatitis C virus (HCV) infection has been found to cause rheumatoid arthritis, even before HCV is detected. Hepatitis C can contribute to liver failure but is also known to cause rheumatoid arthritis – inflammation of the joints. Due to the link between HCV and rheumatoid conditions, it’s important that newly diagnosed patients of rheumatoid conditions also get tested for HCV as rheumatoid conditions can still occur before HCV is even detected.
A rheumatoid disease can be caused by HCV due to a related infection. Rheumatoid diseases cause pain in the joints, muscles and connective tissue. Joint swelling and blood vessel inflammation can occur as well. A recent study dove deeper into the connection between HCV and rheumatoid arthritis and uncovered what may link the two. Continue reading…
Bipolar disorder, poor sleep quality trigger negative moods in women
Advertisement
 A study has found that in women with bipolar disorder poor quality sleep is linked with negative, lower mood. Dr. Erika Saunders, chair, department of psychiatry at Penn State College of Medicine, said, “Patients with bipolar disorder often suffer with sleep problems even when many of their other symptoms are well-controlled. Improving their sleep could not only better their quality of life, but also help them avoid mood episodes.”
A study has found that in women with bipolar disorder poor quality sleep is linked with negative, lower mood. Dr. Erika Saunders, chair, department of psychiatry at Penn State College of Medicine, said, “Patients with bipolar disorder often suffer with sleep problems even when many of their other symptoms are well-controlled. Improving their sleep could not only better their quality of life, but also help them avoid mood episodes.”
“Women and men sleep differently. We know from studies of the general population that women have a different type of sleep architecture than men, and they’re at different risks for sleep disorders, particularly during the reproductive years,” explained Saunders.
Along with sleep differences men and women experience bipolar disorder differently where women often experience more depressive symptoms then men along with co-existing anxiety, eating disorders and migraines. Continue reading…
