 Encephalomalacia is a type of serious brain damage that results in the softening or loss of brain tissue. Causes of encephalomalacia are often linked to inflammation or hemorrhages that are a consequence of being afflicted by cerebral infarction, cerebral ischemia, infection, craniocerebral trauma, or another injury.
Encephalomalacia is a type of serious brain damage that results in the softening or loss of brain tissue. Causes of encephalomalacia are often linked to inflammation or hemorrhages that are a consequence of being afflicted by cerebral infarction, cerebral ischemia, infection, craniocerebral trauma, or another injury.
The term, encephalomalacia, is often used upon gross pathological inspection, as it is much easier to better describe blurred cortical margins and decreased consistency of brain tissue, or brain softening.
Advertisement
Softening may be seen in a localized area or be widespread, depending on the underlying cause. It can affect virtually any part of the brain, possibly damaging tissues of the frontal, occipital, parietal, and temporal lobe. This can present with several motor and sensory deficits.
What causes encephalomalacia?
Stroke
Considered the most common cause of encephalomalacia, strokes occur due to the interrupted blood supply to the brain either through a lack of blood supply to brain tissue or due to hemorrhage of a brain blood vessel. Oxygenated blood is vital for the function and maintenance of brain cells, which will become damaged or die if the blood supply is not promptly restored.
Abnormal accumulation of blood
Occurs when the flow of blood in the brain has become interrupted. This may be due to abnormal brain swelling or the removal of brain tumors resulting in brain damage.
Scar tissue
Damage to brain tissue due to conditions such as a stroke can result in the formation of scar tissue. This area of tissue undergoes contractions and eventually forms encephalomalacia within the brain
Traumatic brain injury
Blunt force trauma to the skull will lead to contusions and possibly brain damage if the force is strong enough. Other forms of penetrating trauma, like from a knife or bullet to the skull, may also lead to the development of encephalomalacia
Other causes
Encephalomalacia may also be the result of:
- Degeneration of the brain
- Deterioration of the brain
- Cerebral stroke or infection
- Blocked blood supply to the brain
- Cerebral ischemia
- Biological pathogens that release chemical toxins that infect the brain
- Leptomeningeal cysts
- Surgery
What are the types of encephalomalacia?
Polioencephalomalacia
Also known as cerebrocortical necrosis (CCN), this neurological disease is caused by the disruption of thiamine production. Thiamine is a B vitamin (B1) and a key chemical in glucose metabolism. If a person were to become deficient in thiamine, significant side effects are likely to develop. The most threatening of which is the inhibition of neurological activity. Polioencephalomalacia will result in damage to the gray matter of the central nervous system, where the majority of information processing takes place. Essential functions like speech, muscle control, memory, and sensory perception can be affected.
Leukoencephalomalacia
A type of encephalomalacia that primarily affects the white matter of the brain. White mater is primarily responsible for ensuring communication between the various parts of the brain and with grey brain tissue. White matter is known for maintaining involuntary actions of the body, which include breathing, heart rate, body temperature regulation, and blood pressure. The development of leukoencephalomalacia can result in the impairment of any of these functions.
Types
There are three types of encephalomalacia, which indicate three levels of brain damage. They are as follows:
Red softening
Commonly seen in cases of hemorrhagic stroke and occurs in regions where brain tissue has become red due to blood in the area where there previously wasn’t.
White softening
Occurring due to a lack of blood supply to the affected region of the brain, giving it a pale white or yellowish appearance. This is often a sign of ischemic damage indicating the imminent damage or death of brain cells.
Yellow softening
Commonly seen in trauma victims, the appearance of yellow-appearing brain tissue is indicative of plaque build-up in the arteries of the brain.
Symptoms of encephalomalacia
Like any cause of damage to the brain, the signs and symptoms will greatly depend on the area of the brain affected. This may lead to the decline of function on one side of the body or maybe even the loss of pain and temperature sensation. However, early signs of encephalomalacia may present similarly regardless of the area of the brain damage.
These symptoms can include:
- Severe headaches
- Head-spinning sensation and vertigo
- Memory loss and mood swings if the frontal lobe is affected
- Clumsiness and diminished coordination
- Visual impairment that may be permanent or temporary
- Extreme drowsiness
Symptoms can vary from person to person, often presenting in unique ways depending on the severity and extent of the damage. Extreme cases of encephalomalacia may potentially even lead to terminal coma, depending on the area of brain softening.
Diagnosing encephalomalacia
Encephalomalacia will often be diagnosed after a particular injury to the brain has occurred, such as a stroke or injury. Various imaging tests will be ordered to help verify its presence. These will include:
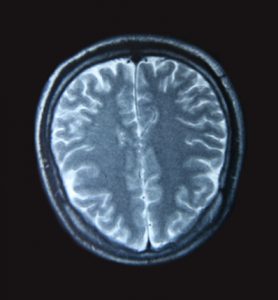
Computerized tomography (CT) scan: A non-invasive imaging test that is a good way to visualize soft brain tissue. It is done by taking a series of x-ray images of the brain at different angles.
Magnetic resonance imaging (MRI): Another non-invasive imaging test that is considered to produce the most detailed images of the brain. The test uses strong radio waves and magnetic fields to produce an image of internal structures of the body.
Encephalomalacia treatment
Brain tissue is non-regenerative, meaning that once it is gone, it’s gone forever as it is unable to rebuild itself after it has become damaged. This is why the brain is considered so important. This makes the primary focus of brain damage treatment to reduce further damage or to prevent it from occurring in the first place.
Encephalomalacia treatment will often involve the following:
- Determining any underlying conditions that lead to these changes in brain tissue
- Removal of damaged brain tissue in severe cases. However, there is no guarantee of the return of bodily function
- Stem cell therapy
Complications and prevention of encephalomalacia
This condition is considered extremely serious and will require the immediate attention of a trained medical professional who specializes in the study of the brain—a neurologist. If left untreated, complications of encephalomalacia may include functional disability, seizures, coma, and even death.
Unfortunately, there is no practical way of preventing encephalomalacia, as it’s not possible to know exactly when you may suffer from severe head trauma or when a stoke will strike. However, you may try your best to avoid these scenarios, which will give you the best chances of avoiding the condition, but there is no sure-fire way.
Advertisement
Related:
What causes blood clots in the brain?
Essential oils for circulation: 10 best oils to improve blood circulation
