 Crohn’s disease and ulcerative colitis are part of the group of conditions known as inflammatory bowel diseases (IBD). Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development – although the exact cause is still unknown.
Crohn’s disease and ulcerative colitis are part of the group of conditions known as inflammatory bowel diseases (IBD). Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development – although the exact cause is still unknown.
For those living with IBDs, their immune system mistakes food and bacteria in the gastrointestinal tract for an allergen or foreign substance, so it sends out cells to destroy it. The result of these attacks is chronic inflammation.
Advertisement
Although the exact causes of Crohn’s disease and ulcerative colitis are unknown, genetics and environmental factors are believed to play a role. Crohn’s disease and ulcerative colitis are often interchanged for one another, but we will outline the differences between the two, including symptoms, causes, and treatments in order to provide you with a better understanding of either condition.
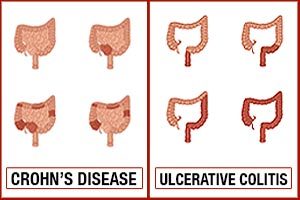
Despite appearing similar to each other, each condition affects the bowel in different locations and is considered a different diagnostic criterion. Ulcerative colitis only affects the inner lining of the large intestine known as the colon. This differs from Chron’s disease as inflammation can occur anywhere along the digestive tract. This means that the signs of the disease may appear any from the mouth to the anus, as well as having areas between inflamed spots called “skip lesions.” Additionally, Crohn’s disease is a more serious condition as it affects all the layers of the bowel walls, not just the inner lining.
Connection between Crohn’s disease and ulcerative colitis
At first, Crohn’s disease and ulcerative colitis will appear the same as they do share many symptoms. This can make diagnosis right off the bat quite difficult until further investigation and testing is underway. Shared symptoms seen across many IBDs include diarrhea, rectal bleeding, urgent need to release bowels, abdominal cramps and pain, sensation of incomplete emptying, constipation, fever, loss of appetite, weight loss, fatigue, night sweats, and loss of menstrual cycle. Recognizing any of these early symptoms can prompt you to speak to your doctor about a possible IBD.
The biggest connection between Crohn’s disease and ulcerative colitis is that they both involve an abnormal response by the body’s immune system. The immune system’s role is to protect the body, but in inflammatory bowel disease this response in abnormal, thus attacking whatever enters the gastrointestinal tract whether it is good or bad. Over time, if treatment is not administered long-term damage can occur to the digestive system and the risk of serious complications arises.
Ulcerative Colitis vs Crohn’s Disease: Distinguishing the Factors
The following table highlights the similarities and differences between Crohn’s disease and ulcerative colitis.
| Factor | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Distribution | Affects small bowel and large bowel | Affects large bowel only |
| Endoscopy findings | Rectum frequently spared Inflammation not continuous (presence of skip lesions) Bowel wall is thickened and has a ‘cobblestoned’ appearance due to deep ulcers and swelling of the tissue | Rectum always affected Inflammation is uniformBowel wall is thin with loss of vascular pattern (blood vessels not visible) |
| Radiology | Strictures are common Deep fissures and fistulae are common Asymmetrical inflammation | Strictures and fissures are much less common Symmetrical inflammation |
| Histology | Presence of granulomas are almost diagnostic Inflammation extends through the mucosa and muscle of the bowel The increase in white cells that tend to be lymphocytes | Granulomas absent Inflammation usually confined to mucosa The increase in white cells that tend to be polymorphs |
| Diet | Remission achieved with enteral feed followed by exclusion/ elimination diet | Unaffected by diet |
| Clinical appearance | Patients often thin and may be malnourished due to intestinal malabsorption of nutrients Diarrhea – only sometimes with blood Abdominal mass common | Weight loss usually related to the severity of active disease Bloody diarrhea Abdominal mass uncommon |
| Smoking | Strongly associated with smoking Predicts a worse course of disease Increases risk of surgery | Associated with non-smokers or ex-smokers Appears to protect against disease |
Crohn’s disease vs. ulcerative colitis: U.S. prevalence and incidence rate
The CDC estimated that one to 1.3 million Americans is affected by IBD. Generally, ulcerative colitis is found to be more common in males where Crohn’s disease is more common in females. Prevalence of Crohn’s disease in the U.S. is 26 to 199 per 100,000 persons, and ulcerative colitis is 37 to 246 per 100,000 persons.
Incidence rate of Crohn’s disease is 3.1 to 14.6 cases per 100,000 person years, and for ulcerative colitis it is 2.2 to 14.3 cases per 100,000 person years.
Distinguishing between Crohn’s disease and ulcerative colitis signs and symptoms
 In either disease, symptoms can range from mild to severe and can even occur as flare-ups if not well managed. Although primary symptoms of Crohn’s disease and ulcerative colitis affect the gastrointestinal tract, other symptoms may also occur, affecting other parts of the body.
In either disease, symptoms can range from mild to severe and can even occur as flare-ups if not well managed. Although primary symptoms of Crohn’s disease and ulcerative colitis affect the gastrointestinal tract, other symptoms may also occur, affecting other parts of the body.
Both conditions often share the following symptoms:
- Belly cramps and pain
- Diarrhea
- Constipation
- An urgent need to have a bowel movement
- Feeling like your bowel movement wasn’t complete
- Rectal bleeding
- Fever
- Smaller appetite
- Weight loss
- Fatigue
- Night Sweats
- Problems with your period. You might skip them, or their timing might be harder to predict.
However, each has its own unique characteristics as well. Crohn’s disease, for example, can affect nearly any tissue found in the digestive tract, going from the mouth all the way to the anus. Ulcerative colitis, on the other hand, only affects the large colon. Inflammation is a common feature of both, but ulcerative colitis tends to have more uniform and uninterrupted lesions as opposed to Crohn’s disease, which can have healthy areas in between inflamed spots. Additionally, ulcerative colitis is more often associated with rectal bleeding and blood in the stool.
Difference between Crohn’s disease and ulcerative colitis causes
As with many autoimmune diseases, the exact cause of either Crohn’s disease or ulcerative colitis is unknown. Some theorized causes of Crohn’s disease include the immune system being triggered by a virus or bacteria, and heredity as many patients with Crohn’s disease will also have a relative with the condition.
The immune system is also suspected to play a role in ulcerative colitis along with genetics and environmental factors. There seems to be some genes involved in the development of ulcerative colitis, and having more than four family members with ulcerative colitis increases your risk of developing it. Environmental factors include place of residence, especially because there appear to be higher rates of ulcerative colitis in urban areas, North America, and Western Europe. Air pollution, medications, and consuming certain diets have also been found to be associated with a higher risk of ulcerative colitis.
Crohn’s disease and ulcerative colitis differences in risk factors and complications
 Risk factors for Crohn’s disease include being aged under 30, being white or of Jewish descent, having family history of Crohn’s disease, smoking cigarettes, using nonsteroidal anti-inflammatory medications, and living in an urbanized area where you eat a high-fat diet or plenty of refined foods.
Risk factors for Crohn’s disease include being aged under 30, being white or of Jewish descent, having family history of Crohn’s disease, smoking cigarettes, using nonsteroidal anti-inflammatory medications, and living in an urbanized area where you eat a high-fat diet or plenty of refined foods.
Ulcerative colitis risk factors are having a family history of colitis, being Caucasian, and taking certain medications such as Accutane, Amnesteem, Claravis, or Sotret.
If not well managed, both Crohn’s disease and ulcerative colitis can progress into complications. Complications associated with Crohn’s disease include inflammation, which can cause the bowel to narrow, bowel obstructions, ulcers, fistulas, anal fissures, malnutrition, colon cancer, osteoporosis, gallbladder, liver disease, and anemia.
Complications that can arise in ulcerative colitis are colon cancer, thickening of the intestinal wall, blood infections, severe dehydration, rapidly swelling colon, liver disease, intestinal bleeding, kidney stones, hole in the colon, ankylosing spondylitis (inflammation of joints between the spinal bones), and inflammation of skin, joints, and eyes.
Crohn’s disease vs. ulcerative colitis: Diagnosis and treatment
Crohn’s disease is diagnosed through a detailed examination of one’s medical and family history, as well as additional testing as needed.
Because Crohn’s disease can mimic other conditions like infections, diverticulitis, and cancer, it’s important to rule them out. Blood tests are ineffective in diagnosing Crohn’s disease, so an ultrasound, CT scan, MRI, colonoscopy, and internal biopsy may be conducted.
Crohn’s disease has a long list of treatment methods because it does not have an exact cause to target. Treatment for Crohn’s disease may include corticosteroids, anti-inflammatory drugs, immunosuppressant agents, antibiotics, biologic agents, nutritional and dietary counseling, stress management, and, in severe Crohn’s disease cases, surgery to remove heavily affected areas of the intestines and colon.
Since some ulcerative colitis symptoms are similar to Crohn’s disease, it is important to get a thorough examination and diagnosis. Ulcerative colitis diagnosis is conducted through a number of tests. Essentially, it is a process of eliminating other conditions. If your doctor suspects an inflammatory bowel issue, they may conduct one or more of the following:
- Stool tests
- Endoscopy – a flexible tube is used to examine the small intestine
- Colonoscopy – a flexible tube inserted into the rectum to examine the colon
- Biopsy – an examination of tissue removed from the colon, likely during colonoscopy
- Barium enema – X-rays taken of colon and rectum, using barium to provide contrast.
- Blood tests – to check for low blood count and C-reactive proteins.
If a diagnosis of ulcerative colitis is confirmed, the doctor will discuss the best possible treatment options. Ulcerative colitis treatment can involve drug therapy, surgery, or in cases where the condition is mild, it can simply mean lifestyle changes.
Advertisement
In some instances, medications are prescribed to help reduce inflammation. Reducing the inflammation can minimize both abdominal cramps and diarrhea. Serious inflammatory bowel disease may require antibiotics or other medications to alter immune function.
When symptoms of ulcerative colitis are severe, hospitalization may be necessary. Oftentimes, severe cases lead to dehydration and malnutrition. Severe symptoms could be a sign of a perforated colon or even cancer. Surgery may be required. There are two surgical options. One, called aprotocolectomy, involves removal of the entire colon and rectum. The other involves removal of part of the colon. This is called ileonal anastomosis. When aprotocolectomy is performed, a surgeon makes a small opening in the abdominal wall to bring the tip of the lower small intestine through the skin’s surface. Waste is then drained through the opening into a bag. With the ileonal anastomosis, feces can still pass through the rectum since the rectum is intact, but the movements will be frequent and watery.
If ulcerative colitis goes undiagnosed and untreated, inflammation can spread, causing problems with other organs and potentially leading to cancer, so proper care and treatment are vital.
