Mild diverticulitis can be easily treated with a proper diet. However, in cases of recurring and severe diverticulitis, surgery may be required.
Diverticulosis, on the other hand, is the presence of multiple diverticula in the colon, resulting from long-time consumption of low-fiber diet. Similar to diverticulitis, diverticulosis is mainly seen in persons over the age of 40 and becomes far more common with age.
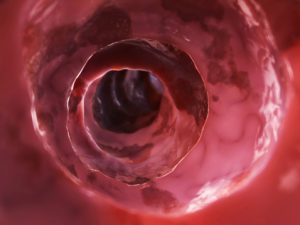
Here we will outline the differences and similarities between diverticulitis and diverticulosis, and how either condition affects the colon.
Diverticulitis vs. diverticulosis: U.S. prevalence
Roughly, two million people in the U.S. suffer from diverticular disease. Prevalence rate is one in 136, or 0.74 percent. Annually, 300,000 new cases of diverticulitis are diagnosed.
Diverticulosis first began appearing in the 1990s in the U.S. as a response to an influx of processed foods. Because of the increased consumption of processed food items, many people’s intake of fiber lowered significantly.
Nearly half of American seniors aged 60 to 80 have diverticulosis, and the prevalence is roughly two million.
Comparing diverticulitis and diverticulosis signs and symptoms
Majority of patients with diverticulosis are asymptomatic, meaning they do not exhibit any symptoms. Fifteen to 25 percent experience symptoms as a result of disease progression into diverticulitis, and 10 to 15 percent will experience painless bleeding. Therefore, in diverticulosis, symptoms only arise when inflammation is present and the condition progresses into diverticulitis.
Difference between diverticulitis and diverticulosis causes
Weak spots along the bottom of the large intestine can prompt the formation of diverticula. When pressure is added, bulges form. These bulges, or pouches, may protrude through the colon wall. When they burst or get infected, this marks the diagnosis of diverticulitis. It is worth noting that diverticula themselves do not necessarily create symptoms.
The main cause of diverticulosis is pressure on the intestinal wall from inside the intestine. This can come with aging, because the outer wall of the intestine becomes thicker over time, causing spaces inside the intestine to narrow, so stool begins to move more slowly through the intestine to the colon.
Hard stools are a result of low-fiber diets, which also contributes to slower transit time – the time it takes for the stool to pass through. Frequent straining during bowel movements adds to the pressure against the intestinal wall, thus causing diverticulosis.
Diverticulitis vs. diverticulosis: Risk factors and complications
Complications that can arise from diverticulitis include the development of an abscess, a blockage of the colon or small intestine, the formation of fistulas, and peritonitis – if the inflamed pouches rupture spilling intestinal contents into the abdomen.
The main complication resulting from diverticulosis is the progression to diverticulitis, which occurs when the diverticula become inflamed.
Diagnosis for diverticulitis and diverticulosis
To properly diagnose diverticulitis, your doctor will conduct a physical examination, checking your abdomen and pelvic region. Other tests include blood tests, pregnancy test for women, liver function tests, stool tests, and CT scans, which can help gauge severity of diverticulitis.
Diverticulosis is diagnosed using one of three tests: barium examination, colonoscopy, or CT scan. In a barium examination, the doctor puts liquid material through the colon and completes an X-ray of the colon, which helps identify diverticula, large polyps, or other growths.
Differentiating diverticulitis and diverticulosis treatment
If diverticulitis is causing pain, there are home remedies you can try for relief. To reduce muscle cramping caused by diverticulitis, you can apply heat to the abdomen. Meditation, too, may be beneficial in managing the associated pain. Lastly, if you need to opt for a pain reliever, stay away from ibuprofen (Advil) and instead reach for acetaminophen (Tylenol).
There are also some preventative measures you can try to lower your risk of developing diverticulitis.
Regular exercise, in particular, is beneficial for preventing diverticulitis because it helps keep bowels regular and reduce pressure on the colon. Added pressure on the colon can result in the formation of diverticula.
Fiber, too, is essential for bowel regularity. And in this vein, staying hydrated helps. Although fiber can help you stay regular, without enough fluids it can have the opposite effect. Staying hydrated improves bodily functions, so it’s important to drink enough water.
The best method to treat diverticulosis is through a healthy diet and constipation relief to avoid complications. The treatment methods, exercise and diet, suggested for diverticulitis can also be used in diverticulosis to prevent its progression into diverticulitis. Therefore, you should bulk up on your fiber, increase your physical activity, and reduce your intake of animal fats and processed food.
By practicing healthy habits, such as eating a balanced diet, exercising, and not smoking, you can reduce your risk of developing diverticulitis and diverticulosis. Although you can’t control aging or turn back the time, you can control these conditions – and it’s as simple as living well.