 Lyme disease and lupus both start with the letter L, and that’s not the only aspect they share. In fact, many Lyme disease symptoms may present themselves as lupus and vice versa. That’s why it’s important to be aware of their distinct differences in order to properly treat either condition.
Lyme disease and lupus both start with the letter L, and that’s not the only aspect they share. In fact, many Lyme disease symptoms may present themselves as lupus and vice versa. That’s why it’s important to be aware of their distinct differences in order to properly treat either condition.
Lyme disease is caused by a tick bite, which transmits bacteria causing infection. Lupus, on the other hand, is a chronic inflammatory autoimmune condition, meaning that the immune system attacks itself and other organs in the body.
Advertisement
In both Lyme disease and lupus, a distinctive rash can appear and both conditions can result in pain as well. Here is a more detailed outline of Lyme disease and lupus to help you distinguish between the two.
Connection between lupus and Lyme disease
Lyme disease and lupus share many symptoms, such as atrioventricular block, which can present itself as heart palpitations. Other shared symptoms include joint pain, fever, fatigue, headache, rashes, and central nervous system complications.
Both conditions can affect the knees. Lyme disease can also cause pain in larger joints, while lupus affects the smaller ones. Arthritis can also be seen in both Lyme disease and lupus, leading to joint pain, too.
Fever occurs mainly in the early stages of Lyme disease and during lupus flares. Fatigue, too, is happening in both diseases, but in Lyme disease it may go away with appropriate treatment, and in lupus it is more frequent and can affect up to 90 percent of patients.
Lyme disease vs. lupus: U.S. prevalence and economic impact
 The Centers for Disease Control and Prevention estimates that Lyme disease cases are closer to 300,000 annually in the U.S., taking into account the many cases that go unreported. The reported number of cases is around 30,000. Even the CDC’s estimate may not fully represent the scale of the Lyme disease problem, as eight national surveys put Lyme diseases cases closer to one million. The economic impact of Lyme disease on the U.S. healthcare system is $16,199 per patient or $3.34 billion annually.
The Centers for Disease Control and Prevention estimates that Lyme disease cases are closer to 300,000 annually in the U.S., taking into account the many cases that go unreported. The reported number of cases is around 30,000. Even the CDC’s estimate may not fully represent the scale of the Lyme disease problem, as eight national surveys put Lyme diseases cases closer to one million. The economic impact of Lyme disease on the U.S. healthcare system is $16,199 per patient or $3.34 billion annually.
Estimated lupus cases are around 1.5 million in America and at least one in five individuals worldwide. Lupus affects women aged 15 to 44 more than men. The economic impact of lupus in the U.S. is $12,643 a patient and $8,659 in lost productivity.
Differences between Lyme disease and lupus, signs, and symptoms
We highlighted some of the shared signs and symptoms in both Lyme disease and lupus, and now we will explore the differences between the two.
In lupus, not every patient experiences the same symptoms, but there are some common ones all patients may encounter. Lupus symptoms come on slowly and may be temporary or chronic. Many patients will experience a flare, which is a symptom spike.
Lupus symptoms vary depending on the affected body part or organ. Some common symptoms of lupus include:
- Fatigue and fever
- Joint pain, stiffness, and swelling
- Butterfly-shaped rash on face
- Skin lesions that worsen in sun exposure
- Fingers and toes turning white or blue in the cold or during stress
- Shortness of breath
- Chest pains
- Dry eyes
- Headaches, confusion, or memory loss
The trademark sign of Lyme disease is a rash that appears as a bull’s eye known as erythema migrans. This rash appears in 70 to 80 percent of patients and is located in the area of the tick bite. Other classic signs and symptoms of Lyme disease include fever, headache, muscle aches, and fatigue.
Symptoms of Lyme disease can occur any time from three to 30 days after infection. As a result, one may forget or not recall being bitten by a tick, adding to the confusion when symptoms do present themselves.
Symptoms of Lyme disease may advance in some patients causing severe joint pain, stiff neck, severe headaches, dizziness, shooting pain, changes in heart rhythm, and issues with the nervous system if not properly treated.
Comparing lupus and Lyme disease: causes and transmission
 Lupus is an autoimmune disease, which can be caused by a combination of genetics and environmental factors. Some individuals, it seems, have a predisposition for the development of lupus, and when they encounter something in their environment that triggers lupus, the symptoms arise and the disease becomes active.
Lupus is an autoimmune disease, which can be caused by a combination of genetics and environmental factors. Some individuals, it seems, have a predisposition for the development of lupus, and when they encounter something in their environment that triggers lupus, the symptoms arise and the disease becomes active.
Potential triggers of lupus include exposure to sunlight, having an infection, or taking certain medications such as anti-seizure medications, blood pressure medications, and even antibiotics.
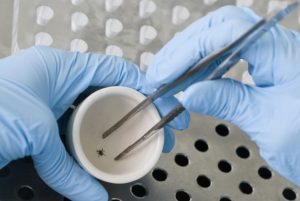
Lyme disease, on the other hand, is caused by the bacteria Borrelia burgdorferi and Borrelia mayonii carried by blacklegged ticks or deer ticks. When a tick bites you, the bacteria get transmitted, and the longer a tick is present on the skin the higher the risk of developing Lyme disease.
Lyme disease vs. lupus: Risk factors and complications
Lupus is an autoimmune disease, so it may not be possible to prevent it completely. Some risk factors that have been found to increase the odds of developing lupus include being a female, being between the ages of 15 to 44, being African American, Hispanic/Latino, Asian American, Native American, Native Hawaiian, or Pacific Islander, and having a family history of lupus. About five to 13 percent of individuals who develop lupus have some family history of the disease.
Because lupus can have an impact all over the body, there are numerous complications that can occur, including kidney damage, kidney failure, complications to the brain and nervous system, resulting in headaches and memory problems, blood problems like anemia, inflammation of the lungs, inflammation of the heart, increased risk of infections, cancer, bone tissue death, and pregnancy complications like miscarriage.
Lyme disease can only be contracted through a tick bite, so a large risk factor is spending time in wooded, grassy areas, especially in the Northeast or Midwest regions of the U.S. If your skin is exposed that can increase the risk of a tick latching on and transmitting the bacteria. Lastly, if a tick is spotted, remove it immediately.
Lyme disease complications include chronic joint inflammation, neurological symptoms, cognitive defects, and heart rhythm irregularities.
Lyme disease and lupus: Diagnosis and treatment options
 Lyme disease is diagnosed by analyzing symptoms, conducting a physical exam, reviewing the patient’s medical history, and running some tests including enzyme-linked immunosorbent assay, western blot, and polymerase chain reaction. These tests check for antibodies and confirm diagnosis.
Lyme disease is diagnosed by analyzing symptoms, conducting a physical exam, reviewing the patient’s medical history, and running some tests including enzyme-linked immunosorbent assay, western blot, and polymerase chain reaction. These tests check for antibodies and confirm diagnosis.
Lyme disease is commonly treated with a regime of antibiotics over the course of several weeks. If Lyme disease is persistent, intravenous antibiotics will be used.
To diagnose lupus, laboratory tests, imaging tests, and biopsies may be utilized. Your doctor may request a complete blood count, erythrocyte sedimentation rate that observes how fast blood cells fall to the bottom of a tube (a fast rate indicates a systemic disease), kidney and liver assessments, urinalysis, and antinuclear antibody test.
Imaging tests include chest X-ray and an echocardiogram to check for fluid in the lung and the heart valves.
Advertisement
There are several treatment options for lupus, including corticosteroids, antimalarials, repository corticotropin injection (which contains the hormone adrenocorticotropic hormone), and aspirin. Other accompanying medications to treat coexisting conditions include diuretics, blood pressure medication, anti-seizure medications, antibiotics for infections, and bone-strengthening drugs to prevent osteoporosis.
Difference in Lyme disease and lupus prevention
Prevention of Lyme disease involves reducing one’s risk of a tick bite. Prevention tips for this include being covered up in wooded, grassy areas, wearing insect repellant, checking yourself, children, and pets for ticks, and removing a tick upon the immediate discovery of one – the longer it stays latched on, the higher the risk of infection.
Because the exact cause of lupus isn’t well understood like in many autoimmune diseases, preventing it completely is hard. What you can do if you have lupus is manage your condition to reduce the risk of flares. This can be done by avoiding triggers like sunlight, paying attention to your diet, exercising regularly, as well as recording your symptoms and documenting what triggers them.
