 You may be wondering, what is pseudogout? Well, you probably have heard of gout, the painful condition that commonly affects the large toe. But pseudogout? While it does sound similar, there are some notable differences.
You may be wondering, what is pseudogout? Well, you probably have heard of gout, the painful condition that commonly affects the large toe. But pseudogout? While it does sound similar, there are some notable differences.
Before we outline the differences between gout and pseudogout, let’s further define pseudogout.
Advertisement
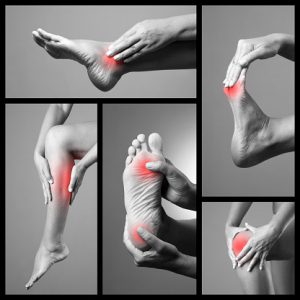
Pseudogout, similar to gout, is an arthritis disease where crystalline deposits form around joints. This formation of crystals can cause pain, swelling, redness, and stiffness of the joint. Unlike gout, which is caused by a build-up of purines, pseudogout is caused by calcium pyrophosphate dihydrate.
Episodes of pseudogout pain can be temporary or last for weeks. Unlike gout, which primarily affects small joints like those found in the big toe, pseudogout is commonly found in the knee.
Causes and risk factors of pseudogout
Pseudogout is caused by the presence of calcium pyrophosphate dihydrate. The formation of calcium pyrophosphate dihydrate crystals can increase with age and it affects nearly half of those over the age of 85. However, many individuals who have these crystals never actually develop pseudogout. It is still unclear why symptoms show in some and not in others.
Risk factors of pseudogout include:
- Older age
- Joint trauma
- Genetic disorders
- Mineral imbalances
- Other medical conditions, such as overactive or underactive thyroid
- Hypercalcemia
- Overactive parathyroid gland
- Magnesium deficiency
- Excess iron
Pseudogout Symptoms
When it comes to symptoms, gout and pseudogout are quite similar. Both conditions cause pain, swelling, and warmth in the affected joint. Pseudogout can also cause redness or a purple color on the skin as well as severe tenderness.
Both men and women can develop pseudogout, but it is more common in women. Pseudogout is also more common in individuals over the age of 60 and in people with thyroid conditions, kidney failure, and in those who have conditions that affect calcium.
Pseudogout is also common in people with osteoarthritis, which can cause a misdiagnosis if both conditions are present at the same time.
How to diagnose pseudogout?
If there is a reason to suspect a diagnosis of pseudogout, your doctor will recommend the following tests:
- Joint fluid analysis: Looking for calcium pyrophosphate crystals, a diagnostic criterion for pseudogout.
- X-rays of the joint: Looking for calcifications (calcium build up) of the cartilage, joint damage, and deposits of calcium in the joint cavities.
Preventing Pseudogout
Preventing pseudogout is challenging. Many of the risk factors are fixed, such as age or genetic disorders. But there are other risk factors that can be adjusted to prevent pseudogout.
Just like maintaining overall good healthy, it is encouraged to enjoy a healthy diet, exercise, and frequent trips to the doctor to keep up to date on your health.
One study even outlined the benefits of consuming coffee and low-fat dairy products in moderation as a means of preventing pseudogout.
Pseudogout Treatment
Advertisement
Treatment for pseudogout can range from natural remedies to medical interventions. Treatment options for pseudogout include:
- Ice the affected joint
- Resting the joint
- Keeping the joint elevated
- Aspiration – a doctor inserts a needle and removes the synovial fluid which accumulated
- Corticosteroid injections
- Oral steroid
- Over the counter anti-inflammatory
- Treating an existing underlying condition
- Surgery
Pseudogout vs. Gout
We have mentioned some similarities and some differences between gout and pseudogout. Here we will further outline what the two have in common and also what makes them different.
| GOUT | PSEUDOGOUT | |
|---|---|---|
| Joint symptoms | Arthritic joint pain, swelling, redness, warmth, in some cases development of tophi, acute onset but chronic condition | Arthritic joint pain, swelling, redness, warmth, extreme tenderness, acute onset but chronic condition |
| Commonly affected joints | Big toe, heels, knees, wrists and fingers | First affects the knees but can move to wrists, ankles, shoulders and other joints |
| Length of symptoms | Five to 12 days but chronic attacks can be longer | Five to 12 days but chronic attacks can be longer |
| Cause | Abundance of uric acid | Abundance of calcium pyrophosphate dihydrate |
| Diagnosis | Imaging tests, fluid drawn from swollen joint, blood test | Imaging tests, fluid drawn from swollen joint, blood test |
| Treatment | Resting joint, icing, painkillers, target uric acid production or excretion, diet low in purines | Resting, icing, painkillers, healthy diet but not strongly associated |
| Prevention | Difficult to prevent, exercise, healthy diet, treating other medical problems | Difficult to prevent, exercise, healthy diet, treating other medical problems |
| Occurrence | Common over the age of 60, common in men, common in those who are obese, in people with kidney problems or hypertension | Common over the age of 60, women more common, can occur with other joint disorders |
Related: Purine-rich foods: Foods to avoid to reduce the risk of gout
